In December 2022, the US biotech firm Moderna, a company that emerged from relative obscurity to become a household name during the pandemic, published the results of a clinical trial that sent ripples through the world of cancer research.
Conducted in partnership with the pharma company MSD, it demonstrated that a messenger RNA (mRNA) cancer vaccine, used in combination with immunotherapy, could offer significant benefit to patients with advanced melanoma who had received surgery to remove their tumours. After a year’s worth of treatment, the phase IIb trial found that the combination reduced the risk of cancer recurrence or death by 44%.
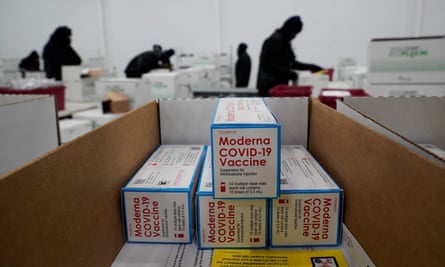
While mRNA has become synonymous with the Covid-19 vaccines developed by Moderna, Pfizer and BioNTech, cancer has long been the ultimate goal of the technology. Now, the NHS has launched a groundbreaking partnership with BioNTech to try and fast-track the development of mRNA cancer vaccines over the next seven years.
As part of the partnership, eligible cancer patients in the UK will get early access to clinical trials from autumn 2023 onwards. The hope is that by 2030, these innovative new treatments can be made clinically available to around 10,000 cancer patients.
This is a remarkable development given that not so long ago, BioNTech’s founders – married entrepreneurs Uğur Şahin and Özlem Türeci – were viewed with suspicion by oncologists as purveyors of a technology that was derided as implausible and impractical.
“I remember in 2012, I spoke publicly about our approach for the first time and after I finished there were no questions,” Şahin says, with a laugh. “Then a pharma executive came to me, and said: ‘Very interesting, but this will never work. If it works, it will never be affordable.’”
Then Covid-19 came along. Suddenly, mRNA was repurposed to make vaccines against the Sars-CoV-2 virus that have since been received by billions of people around the world. Şahin and Türeci became scientific rock stars overnight, profiled by the New York Times and generally receiving the kind of media coverage most executives dream of.
“For us it was a long trip,” says Şahin. “Twenty years ago, people were asking me: ‘Why are you working on mRNA at all?’ It was the ugly duckling, but in 2020, it became the beautiful swan.”
But mRNA cancer vaccines are radically different from conventional vaccines, such as those for Covid-19 and the HPV vaccines that aim to protect against cervical cancer. The focus is not prevention; instead, they are personalised medicines that train the patient’s immune system in how best to fight their own individual cancer. Because time is of the absolute essence, they must be produced in a matter of weeks and they also have to be individually tailored to the unique set of DNA mutations that are driving that patient’s disease.
Moderna and MSD now plan to initiate a phase III trial for advanced melanoma in 2023, while BioNTech expects to release results from its own melanoma trial later this year. Between them, Moderna, BioNTech and CureVac – the third main player in the field – are targeting cancers ranging from ovarian to head and neck, colorectal, lung and even pancreatic.

Ultimately, Şahin foresees two main niches for mRNA cancer vaccines, the first being combination approaches with CAR T-cell or other cell therapies to try to shrink large, rapidly growing tumours and so prolong the lives of patients with advanced forms of the disease who are in danger of dying within a few months. The second niche is in patients who have recently undergone surgery to remove their tumours, to prevent the cancer from recurring and metastasising.
“As an example in colorectal cancer patients, about 30-40% of patients have a relapse after surgery in the first three years,” he says. “But we can give these patients a circulating tumour DNA test, which tells us if there are still cancer cells lingering after the operation and, if it’s positive, those patients will receive the vaccine.”
But while there is considerable optimism surrounding the future potential for these vaccines, there are still some big problems to solve.
Identifying the right targets
Creating a cancer vaccine requires taking samples of the patient’s tumour and healthy tissue, sequencing the DNA and RNA and comparing how these sequences vary between the cancerous and healthy cells to try to identify problem mutations that can be used as antigens or vaccine targets.
This is where the challenge begins: how do you identify the most relevant mutations that are really driving the cancer, a process that is notoriously easier said than done?
“The genomics in the tumour cell are chaotic,” says Prof Alan Melcher from the Institute of Cancer Research. “There’s stuff turning into protein that shouldn’t be turning into protein and there are other places where big chunks of DNA just either get dropped out or inserted or turned around. But at the moment, what we’re missing is how you predict the antigens that matter.”
Researchers believe that this ambiguity is likely to explain some of the variation that is seen in clinical trials, with some patients experiencing clear benefit from vaccines in the context of their disease, while others do not respond so well. Norbert Pardi, an assistant professor at the University of Pennsylvania, says he has seen trials where a vaccine has stimulated the patient’s immune system, but there was little impact on the tumour. “I think this is the most important hurdle that we need to overcome,” he says. “Why don’t we always see benefit in patients even in the presence of a robust immune response?”
When BioNTech and Moderna compare a patient’s tumour cells and healthy cells, they do so by conducting genomic sequencing of the small part of the genome that is related to protein production. This is quicker and cheaper, and their scientists feel that if they can identify abnormal tumour proteins, they should be relatively easy targets for the immune system.
However, with the rapidly falling cost of genome sequencing – the world’s first $100 genome was announced last year – it is becoming more viable to sequence the entire genome. CureVac is already pioneering this approach with the aim of potentially identifying subtler and more hidden targets that relate to how the body’s malfunctioning genetics is enabling the tumour to thrive.
“The tumour genome is full of what are called structural variations,” says Ronald Plasterk, the senior vice-president for science and innovation at CureVac Netherlands. “On average, let’s say in a lung cancer, there’s about 100 to 200 of these structural variations, and they’ve been fully ignored by previous efforts, because you have to sequence the full genome to pull them out.”
But while scientists are still grappling with how best to optimise cancer vaccines against tumours, it may not be long before the first mRNA cancer vaccine hits the market. Moderna and MSD are aiming to launch a much larger phase III trial in advanced melanoma patients this year and, if that proves successful, they could apply for regulatory approval within the next couple of years.
The question then is whether the NHS would be able to afford it.
Can the NHS afford cancer vaccines?
Personalised medicines such as cancer vaccines are by nature extremely expensive, being complex, bespoke products. As a result, while experts say that the UK’s partnership with BioNTech is promising, much work has still to be done to determine whether the cost can be justified for the NHS, should they pass clinical trials.
Christopher Scott, a cancer research professor at Queen’s University Belfast, points out that the current crisis this winter shows just how hard it is proving for NHS staff to deliver the current standard of care, never mind bespoke treatments.
“I remain unconvinced about whether an entirely personalised vaccine approach could be delivered in our NHS,” says Scott. “Because of the Covid vaccines they’ve now got manufacturing processes that have been passed by regulators, which is fantastic, but this is still an expensive technology.”
Melcher is more optimistic but draws parallels with other relatively new cancer medications such as CAR T-cell therapy, which are available on the NHS but only for a very restricted group of patients. CAR T-cell therapies such as tisagenlecleucel – which costs around £282,000 a patient – involve extracting T-cells from the patient’s blood, modifying them and then returning them to the bloodstream. Since 2018, tisagenlecleucel has been available on the NHS just to patients under 25 with B-cell acute lymphoblastic leukaemia, because they are deemed most likely to respond well to the therapy.
However, companies producing mRNA cancer vaccines say that there are a number of steps that are being taken to try to make the process of producing the individualised vaccines as cheap as possible. CureVac has struck a deal with Tesla that will see the electric car manufacturer develop small, portable mRNA bioprinters that could be used to automate the process of producing a patient’s mRNA for their vaccine.
Şahin admits that the cost at the moment is relatively high but he believes it can be brought down once these vaccines are being manufactured for mass numbers of patients. “If you produce personalised vaccines for 1,000 patients per year, it’s a completely different equation compared with producing them for 10,000 or 100,000 patients per year,” he says.
One alternative that is being explored is a more off-the-shelf form of mRNA cancer vaccine. While personalised vaccines are useful for highly aggressive, fast-evolving cancers where it is vital to target a very specific snapshot of the DNA mutations involved, other cancers progress at a slower pace. In these cases, a set of standard antigens, thought to be involved in the disease process across a large number of patients, could be used, making it easier to roll out the vaccine in bulk.
There are still many questions for mRNA cancer vaccines to answer. The next couple of years will provide a lot more information about which cancers they are most effective at tackling – Melcher says that ovarian and pancreatic cancer are much more difficult challenges for a cancer vaccine compared with melanoma due to the nature of the tumours – but there is belief that they can offer new hope to many people suffering from advanced forms of these diseases.
Şahin is bullish that, in one form or another, by the end of the decade we could have many mRNA cancer vaccines routinely available to patients.
“We believe that this will happen on an even broader scale before 2030,” he says. “The Covid-19 vaccine and our expertise in developing it has contributed to our work in oncology. We have learned how to better and faster manufacture vaccines, we have learned about how the immune system reacts to mRNA in a large number of people. And not only have we learned about mRNA vaccines and how to deal with them, but also the regulators, so all this will support the acceleration of the development of mRNA-based cancer vaccines.”

Comments (…)
Sign in or create your Guardian account to join the discussion