The app for independent voices
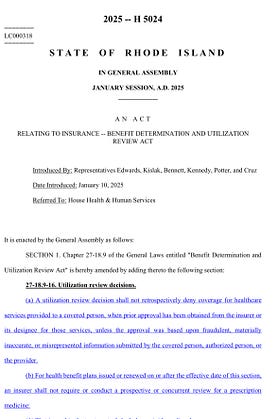
It’s getting to be the time in the legislative session where Committee hearings are packed with both bills and with witnesses waiting to testify. Yesterday’s House Health & Human Services agenda included my bill to eliminate prior authorization requirements for medications used in the treatment of Opioid Use Disorder (OUD).
Prior authorization requirements, for those who are lucky enough to have never experienced them, are one mechanism for insurance companies to protect their bottom lines at the expense of timely and appropriate care. They don’t want to pay for a new, more effective medication (or service), even if the prescriber and patient believe that it is right for the patient’s condition, circumstances, symptoms, etc. Often, they will only approve the necessary medication if the patient has ‘failed’ other types of treatment. Not infrequently, they will recommend an alternative that has been ruled out or is contraindicated for the individual, which the treating prescriber knows.
Forcing someone to ‘fail’ on a medication for OUD can literally be a death sentence. When a treatment is ineffective, individuals may return to use of opioids that are unregulated, unpredictable, and unsafe to alleviate their symptoms. Over 100,000 Americans are dying from overdose every year despite the existence of multiple highly effective medications that can prevent these deaths. There is no excuse for this, but the Managed Care industry has been unchecked for so long that its policies aren’t expected to make sense or be justified.
There is finally evidence of change in this regard. In the HHS Committee last night fourteen bills were heard. Every single one was an effort to reign in MCO power and to put care and funds back in the hands of the people who are actually providing services. In both Senate and House hearings for the OUD Prior Auth bill, a Committee member asked a very informed and pointed question: “After all of the delay and administrative burden, how often is the appropriate medication denied?” The answer is: almost never. This is purely an attempt to discourage providers from getting the best medication to their patients simply to save money for their CEOs and stakeholders.
It’s past time for patients, providers, and elected officials to organize and truly fight back against a system of corporate greed that has been mutating and masquerading as healthcare for the last fifty years. Hopefully we will start with the passage of some of these bills that protect Rhode Islanders.