Abstract
Purpose
The cost of cancer care continues to increase at an unprecedented rate. Concerns have been raised about financial incentives associated with the chemotherapy concession in oncology practices and their impact on treatment recommendations.
Methods
The objective of this study was to measure the physician-reported effects of prescribing chemotherapy or growth factors or making referrals to other cancer specialists, hospice, or hospital admissions on medical oncologists' income. US medical oncologists involved in the care of a population-based cohort of patients with lung or colorectal cancer from the Cancer Care Outcomes Research and Surveillance (CanCORS) study were surveyed regarding their perceptions of the impact of prescribing practices or referrals on their income.
Results
Although most oncologists reported that their incomes would be unaffected, compared with salaried oncologists, physicians in fee-for-service practice, and those paid a salary with productivity incentives were more likely to report that their income would increase from administering chemotherapy (odds ratios [ORs], 7.05 and 7.52, respectively; both P < .001) or administering growth factors (ORs, 5.60 and 6.03, respectively; both P < .001).
Conclusion
A substantial proportion of oncologists who are not paid a fixed salary report that their incomes increase when they administer chemotherapy and growth factors. Further research is needed to understand the impact of these financial incentives on both the quality and cost of care.
INTRODUCTION
Since former President Nixon declared war on cancer four decades ago, the cost of treating cancer has increased dramatically as a result of new diagnostic and treatment technologies and pharmaceutical and biologic treatment innovations. The annual cost of cancer care in the United States exceeded $124 billion in 2010 and is projected to be $173 billion in 2020.1
In addition to the rising cost of initial cancer treatment,2 care is increasingly aggressive near the end of life, with greater use of chemotherapy just before death, more visits to the emergency department, more hospitalizations, and more admissions to the intensive care unit.3–5
Most oncology services are reimbursed as independent units, with separate payments for physician services, diagnostic testing, and chemotherapy administration.6 Thus, similar to most US physicians, medical oncologists' compensation is generally based on their productivity—that is, the more services they provide, the more they bill, and the greater their own individual compensation.7 The practice of medical oncology involves the administration of chemotherapy and supportive medications, such as growth factors, which has led to many private practices having infusion centers in their offices. The chemotherapy concession is the source of approximately 65% of the revenue in a typical oncology practice dwarfing the income from evaluation and management.8 The delivery of chemotherapy in physicians' offices has potential advantages for patients because they may be able to receive treatment in their own community and not have to travel to a hospital for their cancer therapy. However, oncologists who administer chemotherapy in their offices have traditionally charged payers more than their cost for acquiring the drugs, so there is potential for financial conflicts of interest to influence their prescribing behavior.6,9–12 Indeed, it has been suggested that the increased income to physicians from prescribing growth factors has contributed to their widespread adoption.13 Despite these anecdotes from the press, little is known about the actual impact of prescribing chemotherapy or growth factors on medical oncologists' income.
We used survey data from medical oncologists participating in the Cancer Care Outcomes Research and Surveillance (CanCORS) study14 to compare the perceived effects on personal income of administering chemotherapy and growth factors, referring patients to other cancer specialists, referring patients to hospice, and admitting patients to the hospital. In addition, we sought to understand how physician and practice characteristics influence physicians' perception that ordering any of these services would increase their income.
METHODS
Study Design
Data for this study were collected as part of a national study of variations in care and outcomes of care for patients with lung or colorectal cancer undertaken by the CanCORS Consortium.10 CanCORS examined care delivered to population-based cohorts totaling more than 10,000 patients initially diagnosed with lung or colorectal cancer in 2003 to 2005 living in Northern California, Los Angeles County, North Carolina, Iowa, or Alabama or who received care in one of five large health maintenance organizations (HMOs) or 15 Veterans Health Administration (VHA) study sites. Data were collected from patient interviews, medical record abstractions, physician surveys, and surveys of informal caregivers. The study was approved by the human subjects committees at all participating institutions; the investigators obtained informed consent from each participant or each participant's guardian. This analysis uses data only from physician surveys.
Study Population
We surveyed medical oncologists, surgeons, radiation oncologists, and primary care providers named by the patients participating in the CanCORS study as serving important roles in their cancer care from January 2005 through March 2007. Details regarding the physician survey methodology, including characterization of nonresponders, have been published previously.15 This study includes only the medical oncologists who participated in the survey. Of 908 physicians who provided (or discussed) chemotherapy for CanCORS participants for whom contact information was verified, 556 (61%) responded. We included physicians who reported medical oncology as their specialty (n = 495) and excluded respondents who did not respond to the items regarding the outcomes of interest (n = 15), resulting in a final study sample of 480.
Survey Instrument
To understand the physician-reported effects on their personal income of ordering various services or referring patients for various services, medical oncologists were asked “How, if at all, is your income most likely to change as a result of (a) referring more patients to other cancer specialists; (b) enrolling more patients in hospice; (c) admitting more patients to the hospital; (d) enrolling more patients in clinical trials; (e) prescribing/administering more chemotherapy; and (f) prescribing/administering more growth factor (eg, granulocyte colony-stimulating factor).” Response choices included: (1) Likely to increase, (2) Likely to decrease, (3) Not likely to change, and (4) Don't know. Physicians also provided information about personal and practice characteristics, including practice type (characterized as HMO, VHA/government, solo office, single-specialty office group, multispecialty office group, hospital), proportion of patients enrolled in managed care plans, proportion of patients reimbursed on a capitated or prepaid basis, dependence of salary on productivity (asked only of salaried physicians), and among nonsalaried physicians, type of base clinical income (exclusively fee-for-service, predominantly fee-for-service, equal mixture of fee-for-service and capitation, predominantly capitation, and exclusively capitation). An analysis of factors influencing physicians' enrollment of patients in clinical trials has been published separately and is therefore not included here.16
Statistical Analysis
Overall, nonresponse to items was less than 2% to 3% for most variables. We used multiple imputation to impute missing data for these items.17 We dichotomized the response choices into income likely to increase and income not likely to increase, including in the latter category the responses “not likely to change,” “likely to decrease,” and “don't know.”
Since only 1% of physicians reported that their income would be likely to increase with referrals to other cancer specialists or hospice and just 11% reported that income was associated with hospitalizations, these outcomes were not considered in subsequent analyses. We used χ2 tests to assess the association of physician and practice characteristics and the dichotomized response regarding the effect on income of prescribing/administering more chemotherapy and prescribing/administering more growth factors. Specifically, we assessed age, sex, race/ethnicity, board certification, United States or Canadian medical school graduate, teaching involvement, practice type, percentage of patients in managed care, study site, practice at a National Cancer Institute (NCI) –designated cancer center, and physician base payment (salary not based on productivity, salary based on productivity, predominantly fee-for-service, or mixture of fee-for-service and capitation [with at least 50% capitation]). We used logistic regression to estimate the independent associations of physician and practice characteristics with physicians' perceptions that their income would be increased by administering chemotherapy or growth factors.
RESULTS
Just over half the respondents (52%) were age 50 years or older, 23% were female, 78% were graduates of US or Canadian medical schools, 92% were board certified, and 51% were engaged in teaching. Other characteristics of the physicians are delineated in Table 1.
Table 1.
Physician and Practice Characteristics Associated With Self-Report That Referrals or Prescribing Increases Income
| Characteristic | No. of Physicians | % | Physicians Who Report an Increase in Income With Administering: |
|||
|---|---|---|---|---|---|---|
| Growth Factor |
Chemotherapy |
|||||
| % | P | % | P | |||
| Overall | 480 | 25 | 27 | |||
| Physician characteristics | ||||||
| Age, years | .11 | .33 | ||||
| < 40 | 92 | 19 | 20 | 23 | ||
| 40-49 | 135 | 28 | 30 | 31 | ||
| 50-54 | 90 | 19 | 32 | 32 | ||
| 55-59 | 89 | 19 | 19 | 21 | ||
| ≥ 60 | 72 | 15 | 22 | 27 | ||
| Graduate of US or Canadian medical school | .08 | .63 | ||||
| Yes | 377 | 79 | 27 | 28 | ||
| No | 102 | 21 | 19 | 25 | ||
| Sex | .03 | .06 | ||||
| Male | 367 | 76 | 28 | 29 | ||
| Female | 113 | 24 | 18 | 20 | ||
| Race/ethnicity | .32 | .31 | ||||
| Non-Hispanic white | 316 | 66 | 26 | 28 | ||
| Asian | 115 | 24 | 26 | 27 | ||
| Other | 49 | 10 | 15 | 20 | ||
| Board certified in specialty | .11 | .14 | ||||
| Yes | 438 | 91 | 26 | 28 | ||
| No | 40 | 8 | 15 | 18 | ||
| Teaching, days per month | < .001 | < .001 | ||||
| None | 229 | 48 | 36 | 37 | ||
| 1-5 | 148 | 31 | 22 | 25 | ||
| 6 or more | 97 | 20 | 6 | 8 | ||
| Practice characteristics | ||||||
| Type of practice | < .001 | < .001 | ||||
| HMO | 86 | 18 | 5 | 6 | ||
| VHA/government | 46 | 10 | 2 | 4 | ||
| Office | ||||||
| Solo | 52 | 11 | 37 | 52 | ||
| Single-specialty group | 166 | 35 | 49 | 46 | ||
| Multispecialty group | 51 | 11 | 27 | 31 | ||
| Hospital | 79 | 16 | 3 | 6 | ||
| Proportion of patients in managed care, % | < .001 | < .001 | ||||
| ≤ 90 | 372 | 78 | 30 | 32 | ||
| > 90 | 108 | 23 | 11 | 14 | ||
| Practice at NCI cancer center | < .001 | .003 | ||||
| Yes | 97 | 20 | 11 | 16 | ||
| No | 371 | 77 | 29 | 31 | ||
| Physician base clinical payment model | < .001 | < .001 | ||||
| Salary not based on productivity | 203 | 42 | 5 | 5 | ||
| Salary based on productivity | 133 | 28 | 36 | 38 | ||
| All or mostly fee-for-service | 122 | 25 | 46 | 51 | ||
| Fee-for-service with ≥ 50% capitation | 10 | 2 | 38 | 46 | ||
NOTE. No. of physicians missing data on specific characteristics: two, age; one, US medical school graduate; two, board certification; six, teaching status; 12, base clinical payment; 12, NCI cancer center.
Abbreviations: HMO, health maintenance organization; NCI, National Cancer Institute; VHA, Veterans Health Administration.
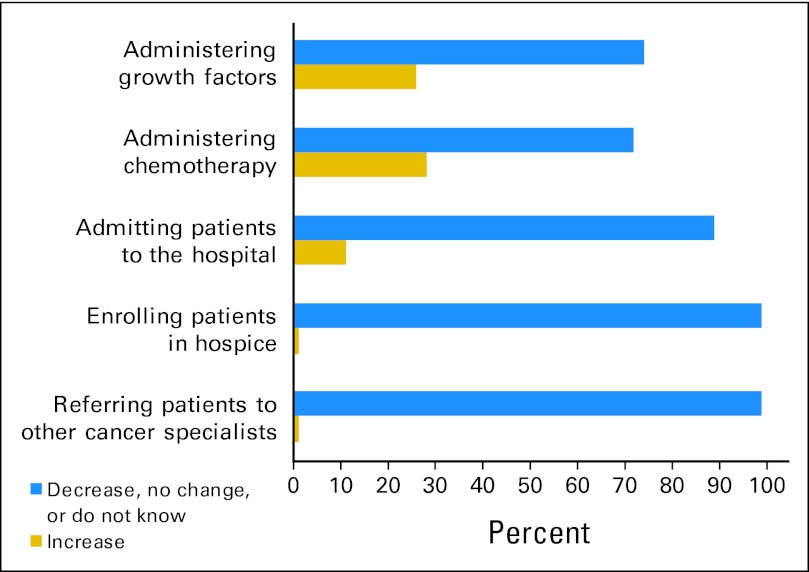
Most medical oncologists reported that their income was unaffected by their prescribing of chemotherapy or growth factors or referrals to other cancer specialists, hospice, or hospital admissions (Fig 1). However, 27% indicated that their income would be increased by administering more chemotherapy, 25% by prescribing more growth factors, and 11% by admitting more patients to the hospital.
Fig 1.
Impact of referrals and prescribing on medical oncologist income.
Although several factors were associated with a greater likelihood of reporting a positive association between income and the two outcomes of interest (Table 1), in multivariate analyses practice characteristics and physician payment models were most strongly associated with income (Table 2). After controlling for payment model and type of practice, the amount of time spent teaching and practicing at an NCI cancer center were no longer associated with increased income for any of the outcomes; however, graduates of US or Canadian medical schools were significantly more likely to report that prescribing growth factors increased their income compared with graduates of foreign medical schools (odds ratio [OR], 2.99; 95% CI, 1.39 to 6.44).
Table 2.
Adjusted Odds of Physician Self-Report That Prescribing Growth Factors or Chemotherapy Increases Their Income (N = 480)
| Characteristic | Administering Growth Factors |
Administering Chemotherapy |
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | |
| Physician characteristics | ||||||
| Age, years | ||||||
| < 40 | 1.0 | 1.0 | ||||
| 40-49 | 1.09 | 0.48 to 2.52 | .83 | 0.87 | 0.40 to 1.88 | .72 |
| 50-54 | 1.41 | 0.58 to 3.47 | .44 | 0.91 | 0.39 to 1.12 | .83 |
| 55-59 | 0.41 | 0.16 to 1.07 | .07 | 0.37 | 0.15 to 0.90 | .03 |
| ≥ 60 | 0.48 | 0.18 to 1.29 | .15 | 0.47 | 0.18 to 1.13 | .09 |
| Graduate of US or Canadian medical school | ||||||
| No | 1.0 | 1.0 | ||||
| Yes | 2.99 | 1.39 to 6.44 | .005 | 1.47 | 0.74 to 2.94 | .27 |
| Sex | ||||||
| Male | 1.0 | 1.0 | ||||
| Female | 0.61 | 0.31 to 1.21 | .15 | 0.69 | 0.37 to 1.31 | .26 |
| Race/ethnicity | ||||||
| Non-Hispanic white | 1.0 | 1.0 | ||||
| Asian | 1.49 | 0.73 to 3.04 | .27 | 0.89 | 0.46 to 1.72 | .73 |
| Other | 0.81 | 0.25 to 2.62 | .72 | 0.71 | 0.25 to 2.08 | .54 |
| Board certified | ||||||
| No | 1.0 | 1.0 | ||||
| Yes | 2.03 | 0.65 to 6.34 | .22 | 1.83 | 0.66 to 5.07 | .24 |
| Teaching, days per month | ||||||
| None | 1.0 | 1.0 | ||||
| 1-5 | 0.67 | 0.37 to 1.21 | .19 | 0.82 | 0.47 to 1.44 | .49 |
| 6 or more | 0.37 | 0.12 to 1.10 | .07 | 0.45 | 0.17 to 1.17 | .10 |
| Practice characteristics | ||||||
| Type of practice | ||||||
| Hospital | 1.0 | 1.0 | ||||
| HMO | 2.40 | 0.38 to 15.38 | .35 | 1.60 | 0.39 to 6.64 | .52 |
| VHA/government | 2.28 | 0.18 to 29.00 | .52 | 2.03 | 0.32 to 12.69 | .45 |
| Office | ||||||
| Solo | 11.28 | 2.08 to 61.30 | .005 | 9.90 | 2.75 to 35.60 | .004 |
| Single-specialty group | 18.76 | 4.00 to 87.93 | .002 | 7.18 | 2.43 to 21.19 | .004 |
| Multispecialty group | 8.31 | 1.62 to 42.63 | .01 | 4.63 | 1.39 to 15.40 | .01 |
| Proportion of patients in managed care, % | ||||||
| < 90 | 1.0 | 1.0 | ||||
| 90 or greater (top quartile) | 1.07 | 0.46 to 2.47 | .88 | 1.04 | 0.49 to 2.23 | .92 |
| Practice at NCI cancer center | ||||||
| No | 1.0 | 1.0 | ||||
| Yes | 0.58 | 0.25 to 1.37 | .22 | 0.92 | 0.43 to 1.98 | .84 |
| Physician base clinical payment model | ||||||
| Salary not based on productivity | 1.0 | 1.0 | ||||
| Salary based on productivity | 5.60 | 2.47 to 12.71 | < .001 | 7.05 | 3.22 to 15.43 | < .001 |
| All or mostly fee-for-service | 6.03 | 2.48 to 13.79 | < .001 | 7.52 | 3.29 to 17.23 | < .001 |
| Fee for service with ≥ 50% capitation | 4.44 | 0.93 to 21.33 | .06 | 7.03 | 1.55 to 31.73 | .01 |
Abbreviations: HMO, health maintenance organization; NCI, National Cancer Institute; OR, odds ratio; VHA, Veterans Health Administration.
Compared with physicians who were paid a salary not based on productivity, the odds of oncologists reporting that their income would increase with administration of chemotherapy were 7.52 (95% CI, 3.29 to 17.23) for those with mostly fee-for-service payment, 7.05 (95% CI, 3.22 to 15.43) for those paid a salary based on productivity, and 7.03 (95% CI, 1.55 to 31.73) for those paid fee-for-service and capitation (with > 50% capitation). Physicians in solo and single-specialty group practice were significantly more likely to report increased income from ordering chemotherapy (OR, 9.90; 95% CI, 2.75 to 35.60 and OR, 7.18; 95% CI, 2.43 to 21.19, respectively) relative to oncologists in hospital-based practices, controlling for all other factors. Similarly, physicians paid on a fee-for-service basis or by salary based on productivity were more likely to report that their incomes increased from prescribing growth factors (OR, 5.60; 95% CI, 2.47 to 12.71 and OR, 6.03; 95% CI, 2.48 to 13.79, respectively). Compared with those in hospital-based practices, oncologists in solo and single-specialty practices were significantly more likely to report a positive association between their incomes and administration of growth factors (OR, 11.28; 95% CI, 2.08 to 61.30 and OR, 18.76; 95% CI, 4.00 to 87.93). Medical oncologists in HMOs or government health care facilities were not significantly more likely than hospital-based physicians to report a positive impact of administering chemotherapy or growth factors on personal income.
DISCUSSION
The results of this study highlight the financial incentives of physicians in the US health care system that may be contributing to rising cancer care costs. A substantial proportion of medical oncologists reported that their income would increase with administering more chemotherapy or growth factors. However, this finding varied tremendously across practice type and physician payment model. In all, 40% to 50% of physicians whose incomes were based on fee for service or who received a salary with productivity incentives indicated that their income increased when they prescribed chemotherapy or growth factors. Physicians in solo single-specialty practice were also much more likely to perceive income increases than physicians in other types of practice settings. These findings for payment model and practice type persisted, even after adjustment for other confounding physician and practice characteristics. The results of this study corroborate and extend the findings from a previous analysis we published18 that used data on the actual prescribing of growth factors for patients treated by physicians in this cohort. It showed that 96% of growth factor use in patients with lung and colorectal cancer occurred in situations in which the chemotherapy regimen did not put them at high risk of febrile neutropenia according to the guidelines and thus represented discretionary use of the therapy. Enrollment in an HMO was strongly associated with a lower adjusted odds of discretionary growth factor use, compared with patients not enrolled in an HMO.
Interestingly, graduates of US and Canadian medical schools were significantly more likely to report financial incentives for prescribing growth factors than graduates of foreign medical schools, even after adjusting for other physician practice characteristics; however, this association was not present for administering chemotherapy. To the best of our knowledge, this difference in perceived financial incentives has not previously been described and the reasons for it are unclear. Some evidence suggests that international medical school graduates may be more likely than other physicians to care for underserved patients, practice in rural areas, and offer volunteer community health care services.19 Differences in cultural values may result in foreign medical school graduates approaching their medical practice with less emphasis on financial success. Alternatively, graduates of international medicals schools may have a lower debt burden when they enter into practice, and this may have an impact on their perception of the financial exigencies of practice.20 This finding underscores the need for further research to elucidate the complex relationship between financial incentives, penalties, and provider behavior.
Because the United States struggles with how best to control health care costs, our results have important implications. Although physician services represent only 20% of health care costs, by ordering health care services, physicians' decisions are responsible for up to 90% of health care expenditures.21,22 With the predominance of the private practice model, most physicians are independent practitioners who bill third-party payers for their services. Although capitation and risk-sharing arrangements have been a heavily relied on approach to control health care costs, we found that few oncologists received a substantial portion of their compensation through capitation arrangements. Nevertheless, these physicians were also more likely than physicians paid by salary not based on productivity to report that their income increased from prescribing chemotherapy. Only salaried physicians without any productivity incentives appeared to be free of financial incentives to administer chemotherapy or growth factors. The fact that physicians who received more than half their income from capitated agreements still had financial incentives to prescribe chemotherapy and growth factors could indicate that pharmacy services are not usually included in risk-sharing arrangements, although it is important to note that only 11 physicians in our cohort reported substantial income from capitation. Capitation schemes that include cancer therapy have not been widely adopted because the high cost of cancer care makes risk-sharing too risky for small practices and because of concerns that such arrangements could lead to withholding of necessary care.23,24 These findings have important implications for accountable care organizations (ACOs), which involve risk-sharing arrangements between hospitals and physicians, currently being advocated as a potential solution to control Medicare costs.25 Our study suggests that ACOs may have little impact on incentives to increase use of cancer services unless the ACO assumes full risk for cancer services and oncologists are reimbursed only for their clinical services or paid a salary.
Beyond a major overhaul of the US health care system, which would be required if all oncologists were to be salaried, how can the financial inducements to administer chemotherapy and supportive care therapies be decreased? Specialty pharmacy programs that provide cancer drugs to the oncologist's office for infusion, thereby eliminating the chemotherapy concession, are one potentially effective strategy, since they remove any financial incentive associated with administering chemotherapy and growth factors. In a recent pilot project, a managed care organization decreased injectable drug costs by 15% by purchasing drugs through a specialty pharmacy program and supplying the drugs to be infused instead of allowing physicians' offices to “buy and bill.”26 However, there are many challenges to successful implementation, including issues related to storage, administration, and concerns about waste if site-of-care laboratory testing indicates that the drug should not be given.27 Another approach that has been proposed involves paying providers for episodes of care (eg, adjuvant therapy for stage III colon cancer) in which the payment would cover all costs of care, including chemotherapy and supportive care drugs.28 The impact of this and other similar approaches on the cost and quality of cancer care is not yet known.
Our results should be viewed in light of several limitations. First, our findings are based on physician self-report of the impact of administering chemotherapy and growth factors on physician income. We do not know whether this accurately reflects the impact of these services on their income, whether and how often oncologists are influenced by this incentive, or the magnitude of this effect. In the most recent National Oncology Benchmark Report,8 practices reported that, on average, 65% of their revenue was from administration of drugs, suggesting that these financial incentives can be substantial. One could argue that such incentives are not necessarily harmful and may in fact be of benefit if they result in more patients receiving high-quality, efficient care. However, as previously mentioned, 96% of growth factor use in the patients cared for by the same physicians included in our analysis was inappropriate according to the guideline recommendations at the time, suggesting that these financial incentives are contributing to waste in the health care system.14 Finally, it should be noted that we did not explore factors that could lead to a decrease in physicians' income. Because the amount that most payers will reimburse for drugs has substantially decreased over the last decade, some oncologists may find that reimbursements for some drugs may not cover their cost. Although only a few respondents to our survey reported that their income would decrease as a result of administering chemotherapy or prescribing growth factors, this may become more of a concern as cost containment efforts continue to exert pressure on reimbursement.
In conclusion, a substantial proportion of oncologists who are not paid a fixed salary report that their income increases when they administer chemotherapy and growth factors. New payments models are needed to counter or eliminate these incentives to decrease unnecessary care and ensure that health care resources are used most effectively.
Acknowledgment
We thank Yang Xu, MS, for assistance with statistical programming.
Footnotes
See accompanying editorial on page 517
Supported by Grants No. U01 CA093344 from the National Cancer Institute (NCI) to the Statistical Coordinating Center, U01 CA093332 from the Dana-Farber Cancer Institute/Cancer Research Network, U01 CA093324 from Harvard Medical School/Northern California Cancer Center, U01 CA093348 from RAND/University of California, Los Angeles, U01 CA093329 from the University of Alabama at Birmingham, U01 CA01013 from the University of Iowa, U01 CA093326 from the University of North Carolina, and CRS 02-164 from the Department of Veterans Affairs (VA) to the Durham VA Medical Center.
The views and opinions of authors expressed herein do not necessarily state or reflect the Department of Veterans Affairs, the United States Government, Kaiser Permanente, or WellPoint.
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Although all authors completed the disclosure declaration, the following author(s) indicated a financial or other interest that is relevant to the subject matter under consideration in this article. Certain relationships marked with a “U” are those for which no compensation was received; those relationships marked with a “C” were compensated. For a detailed description of the disclosure categories, or for more information about ASCO's conflict of interest policy, please refer to the Author Disclosure Declaration and the Disclosures of Potential Conflicts of Interest section in Information for Contributors.
Employment or Leadership Position: Jennifer L. Malin, WellPoint (C) Consultant or Advisory Role: Jennifer L. Malin, Onyx Pharmaceuticals (C) Stock Ownership: None Honoraria: None Research Funding: None Expert Testimony: None Other Remuneration: None
AUTHOR CONTRIBUTIONS
Conception and design: All authors
Collection and assembly of data: Jennifer L. Malin, Jane C. Weeks, Mark C. Hornbrook, Nancy L. Keating
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
REFERENCES
- 1.Mariotto AB, Yabroff KR, Shao Y, et al. Projections of the cost of cancer care in the United States: 2010–2020. J Natl Cancer Inst. 2011;103:117–128. doi: 10.1093/jnci/djq495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Warren JL, Yabroff KR, Meekins A, et al. Evaluation of trends in the cost of initial cancer treatment. J Natl Cancer Inst. 2008;100:888–897. doi: 10.1093/jnci/djn175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Earle CC, Neville BA, Landrum MB, et al. Trends in the aggressiveness of cancer care near the end of life. J Clin Oncol. 2004;22:315–321. doi: 10.1200/JCO.2004.08.136. [DOI] [PubMed] [Google Scholar]
- 4.Earle CC, Landrum MB, Souza JM, et al. Aggressiveness of cancer near the end of life: Is it a quality-of-care issue? J Clin Oncol. 2008;26:3860–3866. doi: 10.1200/JCO.2007.15.8253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sharma G, Freeman J, Zhang D, et al. Trends in end-of life ICU use among older adults with advanced lung cancer. Chest. 2008;133:72–78. doi: 10.1378/chest.07-1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bach PB. Costs of cancer care: A view from the Centers for Medicare and Medicaid Services. J Clin Oncol. 2007;25:187–190. doi: 10.1200/JCO.2006.08.6116. [DOI] [PubMed] [Google Scholar]
- 7.Reschovsky JD, Hadley J. Physician Financial Incentives: Use of Quality Incentives Inches Up, but Productivity Still Dominates. Issue Brief No. 108, January 2007. http://hschange.org/CONTENT/905/#ib6. [PubMed]
- 8.Barr TR, Towle EL. National oncology practice benchmark: An annual assessment of financial and operational parameters—2010 report on 2009 data. J Oncol Pract. 2011;7(suppl 2):2s–15s. doi: 10.1200/JOP.2011.000223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.General Accounting Office. Washington, DC: General Accounting Office; 2001. Medicare: Payments for covered outpatient drugs exceed providers costs. GAO-01-1118. [Google Scholar]
- 10.Elliott SP, Jarosek SL, Wilt TJ, et al. Reduction in physician reimbursement and use of hormone therapy in prostate cancer. J Natl Cancer Inst. 2010;102:1826–1834. doi: 10.1093/jnci/djq417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jacobson M, Earle CC, Price M, et al. How Medicare's payment cuts for cancer chemotherapy drugs changed patterns of treatment. Health Aff (Millwood) 2010;29:1391–1399. doi: 10.1377/hlthaff.2009.0563. [DOI] [PubMed] [Google Scholar]
- 12.Smith TJ, Hillner BE. Concrete options and ideas for increasing value in oncology care: The view from one trench. Oncologist. 2010;15:65–72. doi: 10.1634/theoncologist.2010-S1-65. [DOI] [PubMed] [Google Scholar]
- 13.Berenson A, Pollack A. Doctors reap millions for anemia drugs. New York Times. 2007 May 9; http://www.nytimes.com/2007/05/09/business/09anemia.html?_r=1&scp=44&sq=&st=nyt. [Google Scholar]
- 14.Ayanian JZ, Chrischilles EA, Fletcher RH, et al. Understanding cancer treatment and outcomes: The Cancer Care Outcomes Research and Surveillance Consortium. J Clin Oncol. 2004;22:2992–2996. doi: 10.1200/JCO.2004.06.020. [DOI] [PubMed] [Google Scholar]
- 15.Keating NL, Landrum MB, Klabunde CN, et al. Adjuvant chemotherapy for stage III colon cancer: Do physicians agree about the importance of patient age and comorbidity? J Clin Oncol. 2008;26:2532–2537. doi: 10.1200/JCO.2007.15.9434. [DOI] [PubMed] [Google Scholar]
- 16.Klabunde CN, Keating NL, Potosky AL, et al. A population-based assessment of specialty physician involvement in cancer clinical trials. J Natl Cancer Inst. 2011;103:384–397. doi: 10.1093/jnci/djq549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.He Y, Zaslavsky AM, Landrum MB, et al. Multiple imputation in a large-scale complex survey: A practical guide. Stat Methods Med Res. 2010;19:653–670. doi: 10.1177/0962280208101273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Potosky AL, Malin JL, Kim B, et al. Use of colony-stimulating factors with chemotherapy: Opportunities for cost savings and improved outcomes. J Natl Cancer Inst. 2011;103:979–982. doi: 10.1093/jnci/djr152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bazemore AW, Goldenhar LM, Lindsell CJ, et al. An international health track is associated with care for underserved US populations in subsequent clinical practice. J Grad Med Educ. 2011;3:130–137. doi: 10.4300/JGME-D-10-00066.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gozu A, Kern DE, Wright SM. Similarities and differences between international medical graduates and U.S. medical graduates at six Maryland community-based internal medicine residency training programs. Acad Med. 2009;84:385–390. doi: 10.1097/ACM.0b013e318197321b. [DOI] [PubMed] [Google Scholar]
- 21.Kaiser Family Foundation. U.S. health care costs: Background brief. 2010. Mar, http://www.kaiseredu.org/topics_im.asp?imID=1&parentID=61&id=358.
- 22.Eisenberg JM. Physician utilization: The state of research about physicians' practice patterns. Med Care. 2002;40:1016–1035. doi: 10.1097/01.MLR.0000032181.98320.8D. [DOI] [PubMed] [Google Scholar]
- 23.Zarkowsky H. Oncology services for members of a national managed care company. Cancer. 1998;82:2039–2042. doi: 10.1002/(sici)1097-0142(19980515)82:10+<2039::aid-cncr11>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 24.Butcher L. US Oncology prepares for risk-based contracts. Oncology Times. 2010;32:25–26. [Google Scholar]
- 25.Berwick DM. Launching accountable care organizations: The proposed rule for the Medicare Shared Savings Program. N Engl J Med. 2011;364:e32. doi: 10.1056/NEJMp1103602. [DOI] [PubMed] [Google Scholar]
- 26.Baldini CG, Culley EJ. Estimated cost savings associated with the transfer of office-administered specialty pharmaceuticals to a specialty pharmacy provider in a Medical Injectable Drug program. J Manag Care Pharm. 2011;17:51–59. doi: 10.18553/jmcp.2011.17.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pane FJ. White bagging: A new challenge for your hospital. Pharmacy Practice News. 2009;36:12. http://pharmacypracticenews.com/ViewArticle.aspx?d=Operations+&+Management&d_id=53&i=December+2009&i_id=587&a_id=14378. [Google Scholar]
- 28.Bach PB, Mirkin JN, Luke JJ. Episode-based payment for cancer care: A proposed pilot for Medicare. Health Aff (Millwood) 2011;30:500–509. doi: 10.1377/hlthaff.2010.0752. [DOI] [PubMed] [Google Scholar]