Discover more from Protons 101
PSA Kinetics - Even we get confused.
We've done a poor job simplifying endpoints. Even amongst radiation oncologists, we seem a bit confused. I'll explain...
www.protons101.com
Home to the musings of a radiation oncologist - with a slant on protons and dose and optimizing cancer outcomes.
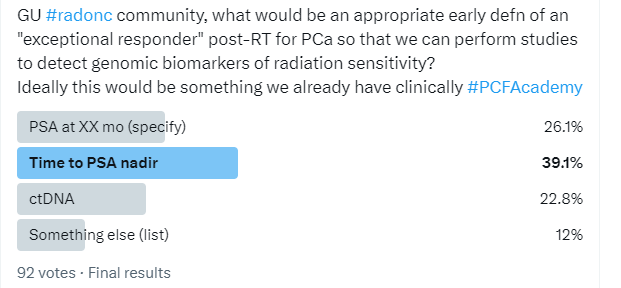
I’ve spent a lot of time talking about PSA kinetics and I want to look at a recent poll from Twitter - honestly a pretty darn well educated group of radiation oncology physicians. Here is the poll:
And the winner is? Time to PSA nadir. It was selected by experts as the appropriate “early definition” for “exceptional responder” after radiation. Today, we’ll look at why I don’t believe this is the answer - in fact, I believe it is clearly incorrect.
So if I interpret the question correctly, I’m left with nearly 40% of people in the field of radiation oncology (or really odd birds on Twitter) missing this on a first impression click? Yikes. So, let’s look at data.
(Author of one: If I’m wrong or missed something, please comment below)
Exhibit 1: One graph will pretty do the work for today. This is 2000 men with SBRT from the Refining the definition of biochemical failure in the era of stereotactic body radiation therapy for prostate cancer: The Phoenix definition and beyond paper published in November of 2021. Blow it up - look at the graph and the numbers.
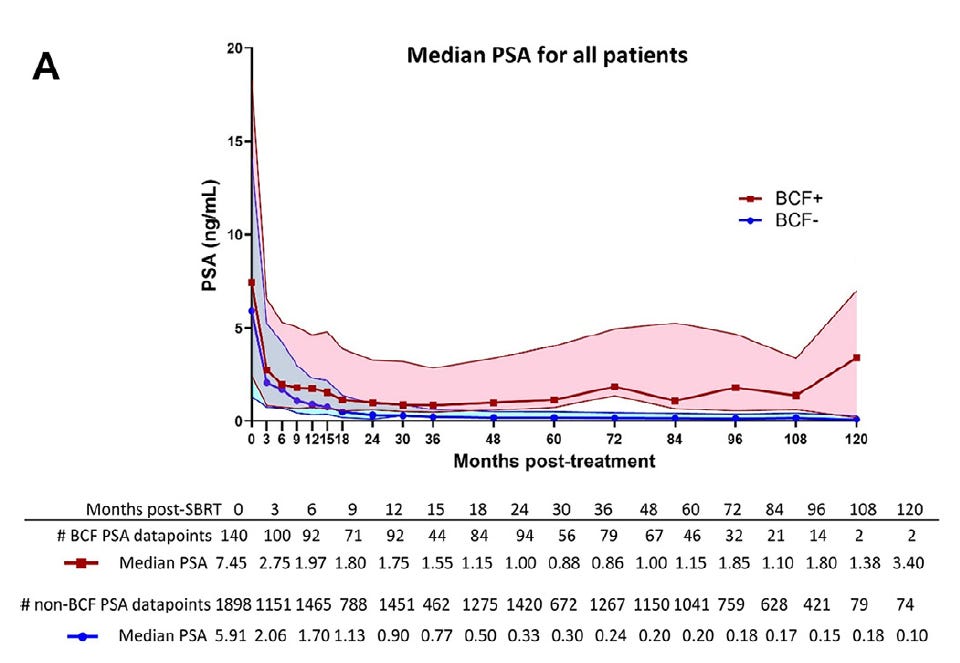
This is a strong series result - 5 year biochemical disease free survival of ~7%. At 10 years, the cured patients STILL have not nadired. The failing patients, in contrast, nadired at 36 months.
If you answered “time to PSA nadir”, you really only have two options: early or late - and both are wrong.
If you thought an early nadir was a good predictor, you are wrong, by at least 7 years. Yes those that nadir early will parse the cohort into the 7% that fail but they are NOT the exceptional responders - quite the contrary. If you think late is answer, you are arguing to wait 10 years - at which point you can only narrow the cohort to about 1/2 of the original patient population. (93% / 2). And for one of those two reasons, some selected “time to PSA nadir” as the “best” “early” predictor of an “exceptional responder”.
I’ll summarize the remainder of our literature:
It is consistent with this large SBRT series.
Yes lower dose, older trials will nadir earlier and higher as more people fail in many series that do not cure as many men, but the trend remains - early nadirs are bad, late nadirs are good. And the question posed is specifically looking to improve our future treatments. So lets at least use good outcome data - and this SBRT represents strong outcome data kinetics. And simply stated, this is how PSA kinetics work across the entire history of our literature.
(In the bottom of the article, I’ll link a few of the stronger articles reviewing kinetic data on this Substack - I bet I’ve read at least 50 kinetics papers this year - and to be fair, PSA kinetics is maybe one single question on a board licensing exam - a tiny detailed piece of our field but maybe after one article one might have a better mental filing system - it is after all one of our largest patient cohorts).
So, at least to me, we seem to have eliminated the most common answer. That doesn’t bode well.
From my perspective, the best ‘answer” in the comments (discounting the one that says “none based on statistical concerns”) relates to this paper: Four-year Prostate-specific Antigen Response Rate as a Predictive Measure in Intermediate-risk Prostate Cancer Treated With Ablative Therapies: The SPRAT Analysis. But even in giving the answer, Dr. Loblaw notes the issue adding quotes around the word “early”.
I’ll summarize the paper: Patients with a PSA of less than 0.4 at 4 years have a really low failure rate, like super low. The paper reports a magical type separation: in 637 patients they report that IF the PSA reached <0.4 at 4 years, the chance of recurrence was 1.7%. But if it was 0.4 or higher, the rate was 27%.
I have no doubt lower is better and different datasets will break different ways, but there is literally no way in a continuous variable that ANY arbitrary data cut-point represents a 16x increase in failure. Did it exist here? Sure - I guess. Will it be reproducible on any level at that margin of benefit - no way. They don’t overstate it in the conclusion - kudos to the authors there. Is it a good number to remember and evaluate? Sure. Any more “valid” than my historical reviews I’ve done on this site? Maybe?, but maybe not.
From my perspective, the paper can unfortunately be used to argue in favor of “none of the above” due to implications that the results / statistics will be misleading or overstated with respect to a finding a genetic biomarker for response. Quite sad, but I find that actually to be quite valid.
Simply ask ChatGPT about issues with this type of approach or here is a highly cited statistical reference from the British Medical Journal (either will do):
The cost of dichotomising continuous variables
Use of this so called “optimal” cutpoint (usually that giving the minimum P value) runs a high risk of a spuriously significant result; the difference in the outcome variable between the groups will be overestimated, perhaps considerably; and the confidence interval will be too narrow. This strategy should never be used.6,7
But I actually like the idea in the initial poll of looking for genetic sensitivity - really strong and appealing to me, but I agree that today, we often can miss translating numbers to clinical benefit. (I know… I know… on a proton named site - quite ironic).
The point of the question was to look for an early market of excellent response - the radiation oncology community offered a 10 year and 4 year answer. Each would get you fired from any pharma development company. To be competitive, we have to iterate FAR faster than anything presented. To me, that is actually the more concerning aspect - perhaps even worse than the lack of understanding of PSA kinetics - the lack of context that our field must be more adaptive. We have to fasten our pace of change. On Twitter our fields answer was? 10 years. Quite funny / ironic. Do great science, but wow - understand and appreciate the context of the competitive marketplace that we operate / radiate in. :) (Teaser to ROCR discussion upcoming).
Me? I think we have good data at 1 year and 2 year marks. Our literature is blazingly consistent. PSA kinetics have been consistent with dose levels over decades from my review of our literature.
Here I presented my recommendations:
<1 at 1yr and <0.5 at 2yrs - mean nadirs.
(Note mean will be higher than median in these datasets and will be far more sensitive to failures - rising much faster. Full rationale for choice in article below):
Prostate Cancer: Using 1yr and 2yr PSA Metrics to Improve Outcomes and Limit ADT
If you don’t like my final assessment look back to the SBRT paper (with the graph). It evaluated that dataset and found a ratio of the PSA (18 months) / PSA (6 months) as part of their recommendation. Ironically, the SPRAT Analysis referenced was published literally 13 days later and it contains many of the same authors. Read both articles. They publish quite divergent answers on a recommended predictive answer - one quite complicated, one simple. It is as if they published the first, weren’t quite convinced, and then ran a second database and come up with a different answer and then published both - in fact, the metric from the “first” paper was not evaluated in the second paper less than 2 weeks later and vise versa.
To me, more than the fault of the common authors, I think that speaks to issues within both academics and the publishing factories that they largely created over the decades - and part of why I’m here - in a different environment on Substack. Even those authors maybe haven’t realized how two different pieces of data from two different projects written by two largely different sets of authors published two different answers less than two weeks apart. Today, it is more about publishing the trees rather than presenting the context of the forest.
I published my goalposts of <1 at 1 yrs and <0.5 at 2 yrs about 4 months ago. To date, I stand by that analysis - a massive improvement upon 2 weeks (sarcasm). And this brings us back to the subtitle: We've done a poor job simplifying endpoints. No wonder our own community is somewhat confused as to what is the best answer is on a quick first impression click. Read those two articles back to back and you too might land on the best answer being in fact: “none of the above due to statistical concerns”.
Me, I’m from Arkansas and like to keep things simple - lower is better. Nothing is magical. Really low really early relates to really good long term cure.
For my answer, I went to my database (around 150 patients without ADT) and wrote this:
Exceptional - say top 10% response. In my database that is 0.3 at 6 months for 7250 and 0.4 at 6 months for 7920. Faster to lower is better - just a matter of picking size of subset. Strongest ultimate predictor of outcome is slight different question.*
I get it - medicine is hard and can be complex. But it ain’t always.
Additional PSA Kinetic Articles on this Substack:
*I did correct a twitter speed typo. :)