
Discover more from Your Local Epidemiologist
This week I’m diving deep into long COVID. We’ve been so focused on the pandemic’s impact on lives lost that we’ve neglected to recognize health lost. This mini-series will be 5 posts in total on long COVID: burden, impact on specific organs, predictors, kids, and treatment. This is #1 post of the series. Buckle up!
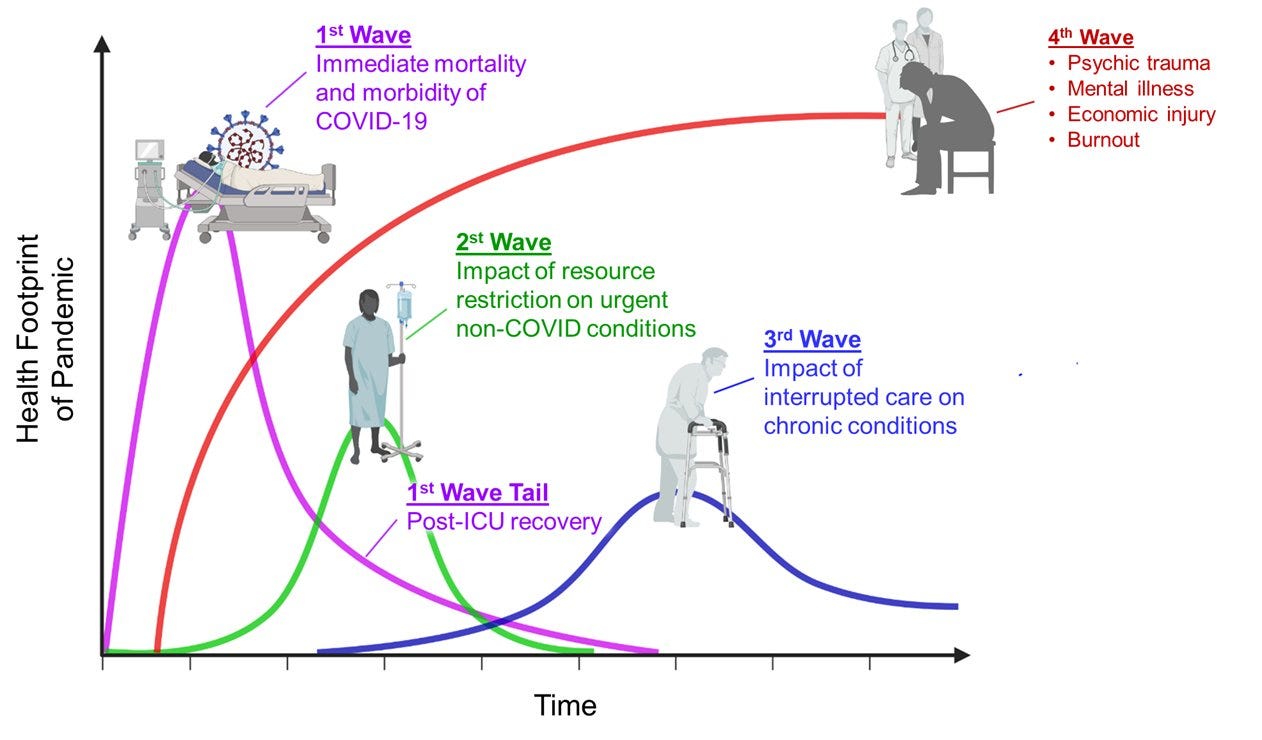
The health footprint of any pandemic typically extends decades after immediate impact. While we may (or may not) be done with immediate disease, the footprint of SARS-CoV-2 will be long lasting. Long COVID will no doubt play a role.
What is long COVID?
Long COVID is also known as long-haul COVID, post-acute COVID-19, long-term effects of COVID, or chronic COVID. To medical professionals it’s known as Post Acute Coronavirus Disease Syndrome (PACS).
Whatever the name, it seems to have become an umbrella term for a constellation of syndromes. It can be further broken down into three categories based on cause:
Direct cell damage. At initial infection, it takes about 10 minutes for SARS CoV-2 to find the doors of your cells (called ACE2 receptors) and make a cell its home. Once in, the virus starts multiplying, eventually killing the cell (and sometimes even killing all the cells in the organ). This initial and direct cell damage can cause lingering or ongoing symptoms. For example, SARS-CoV-2 has shown to directly cause cell damage to the heart, thus leading to long-lasting arrhythmias.
Chronic hospitalization. Lingering symptoms can also be a result of being bed bound for weeks in the hospital. Patients can show muscle weakness, cognitive brain dysfunction, and psychosocial stress. This is not unique to SARS-CoV-2, as this phenomenon occurs during all types of hospitalizations. In the medical world, we call this post-ICU care syndrome.
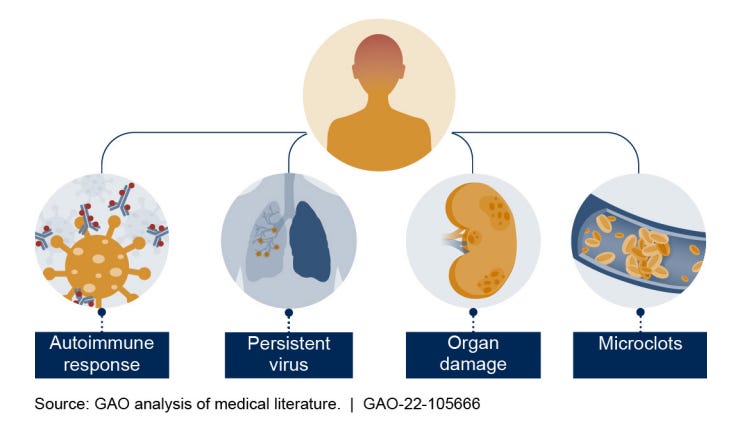
After acute recovery. Then there are symptoms that appear after apparent initial recovery of the virus. We don’t know why this happens, but the scientific community has two leading theories:
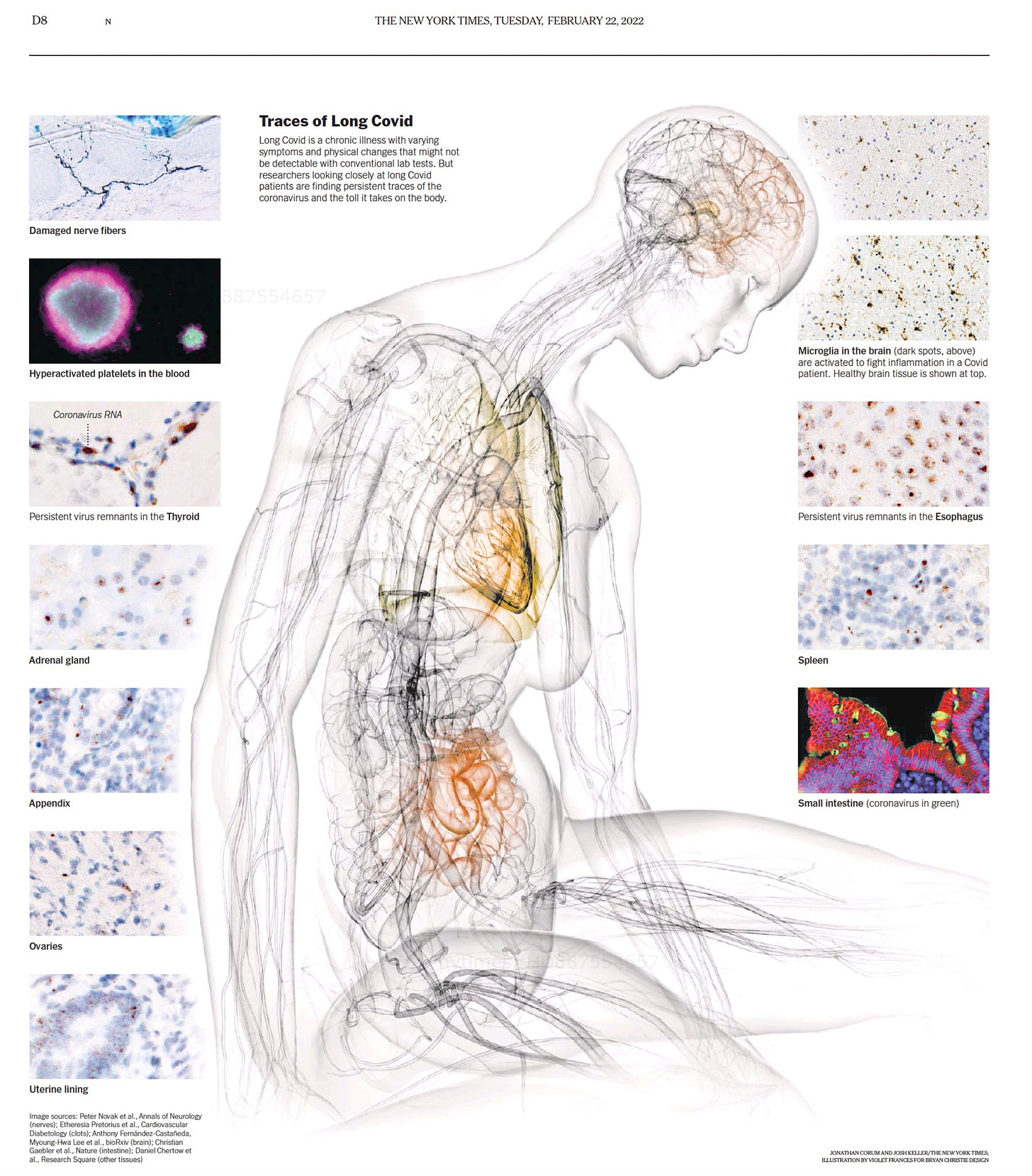
Viral persistence (lingering virus): There has been considerable evidence that some people harbor the virus in their tissue. These viral reservoirs can both cause direct damage to cells and leak viral particles into the blood, where they can create microclots, activate inflammation, and ultimately cause more damage. The figure below from the NYT shows traces of the virus in all types of different tissues, including the esophagus, thyroid, and spleen.
Immune system: The second theory is that long COVID symptoms are driven by the immune system. This can be caused by micro-blood clots (like in the previous bullet), which have been shown to conceal autoantibodies. Then the body starts attacking itself. The other thing that may happen is immune dysregulation. Even if the body cleared the virus, the immune system is off balance, allowing other dormant viruses to reactivate, like herpes or a parasite called Toxoplasma. These then drive chronic symptoms.
In reality, the cause of long COVID for most people is likely a combination of pathways.
How many people have long COVID?
The burden of long COVID has been extremely difficult to grasp. Prevalence and incidence estimates have vastly ranged from 2% to 75%. This is due to three main reasons:
Varying definitions. There still isn’t a consensus for a long COVID definition. On October 6, 2021, the World Health Organization provided a working definition: “Post COVID-19 condition occurs in individuals with a history of probable or confirmed SARS-CoV-2 infection, usually 3 months from the onset of COVID-19 with symptoms that last for at least 2 months and cannot be explained by an alternative diagnosis.” But the CDC and the U.K., for example, define long COVID as symptoms persisting 4 weeks after infection. As a result, studies measuring morbidity come to different burden conclusions.
Different settings. In the beginning stages of discovery, the majority of long COVID studies were among hospitalized patients, which resulted in very high prevalence rates. It’s become increasingly clear that long COVID can also manifest from asymptomatic and mild disease too. Obtaining a generalizable sample continues to be challenging.
Lack of comparison groups. Because we cannot ethically conduct a randomized controlled trial of infections, the next best thing is to use a comparison group to measure prevalence. This is especially important with long COVID, as many symptoms, like fatigue and headache, are common outside of SARS-CoV-2. Rigorous comparison studies are becoming more and more common; however, they take time to do well.
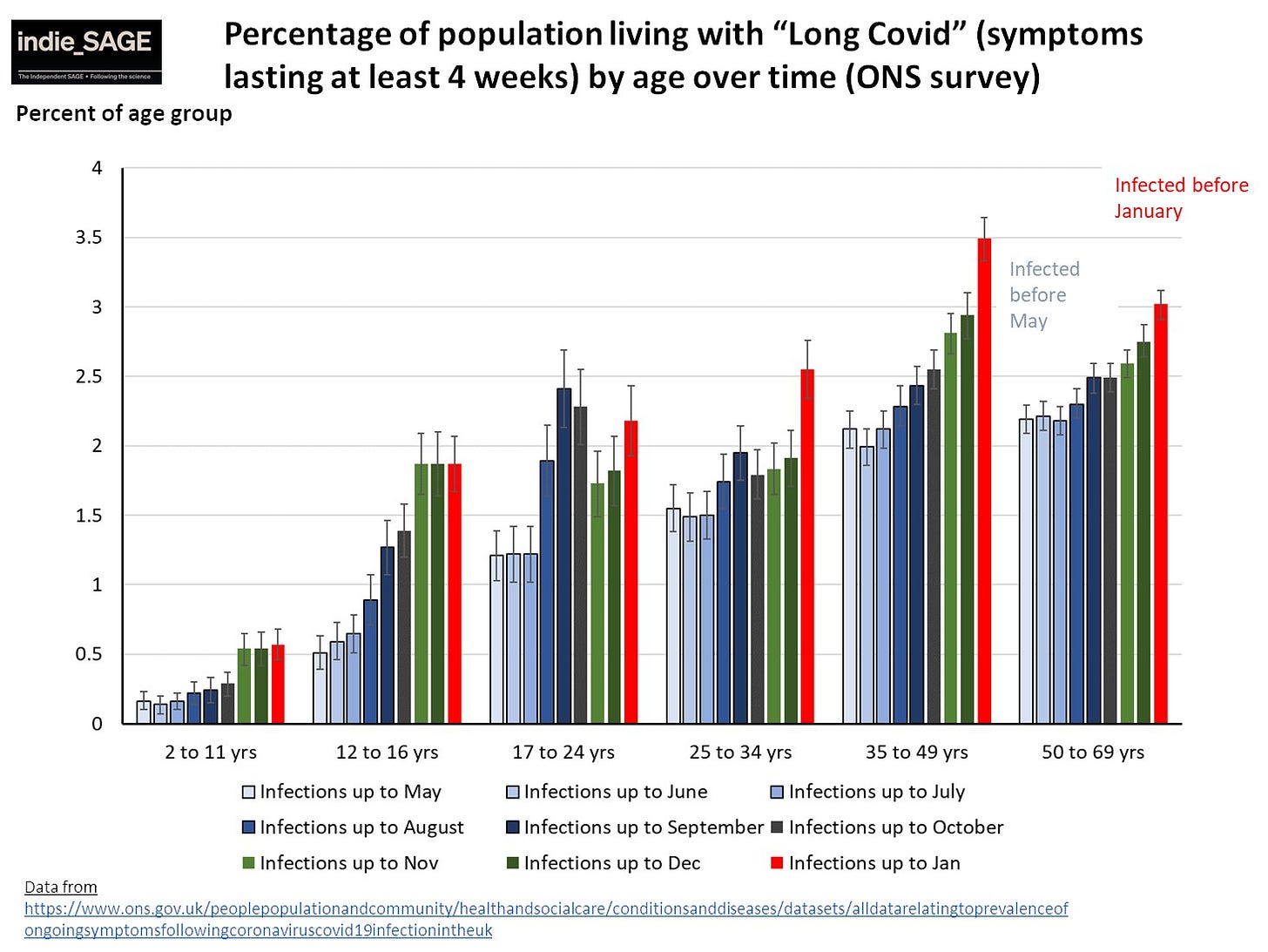
Nonetheless, the American Academy of Physical Medicine and Rehabilitation uses an estimate of 30% on their long COVID dashboard, which equates to 23.44 million Americans currently experiencing long COVID. The U.K. officially estimates a 2.3% burden of long COVID, which would equate to 6 million Americans.
What is clear is that the longer this virus circulates, the higher the burden. Data from the U.K. showed that although disease was, on average, less severe from Omicron, long COVID diagnoses were still alive and well.
Symptoms of long COVID
We have SARS-CoV-2 doors (called ACE2 receptors) on almost all of our organs, which means almost every organ has the potential to be impacted from SARS-CoV-2. This leads to highly variable symptoms of long COVID from one person to the next. In fact, one study found long haulers reported more than 200 symptoms across 10 organ systems.
In a recent Danish study, the most common symptoms within 6 months of infection were loss of smell and taste, exhaustion, labored breathing, reduced strength, pain, difficulty concentrating, and sleep problems. Interestingly, the most common symptoms are different by sex and age. For example, younger people had were more likely to have impaired taste/smell after 6 months compared to older people.
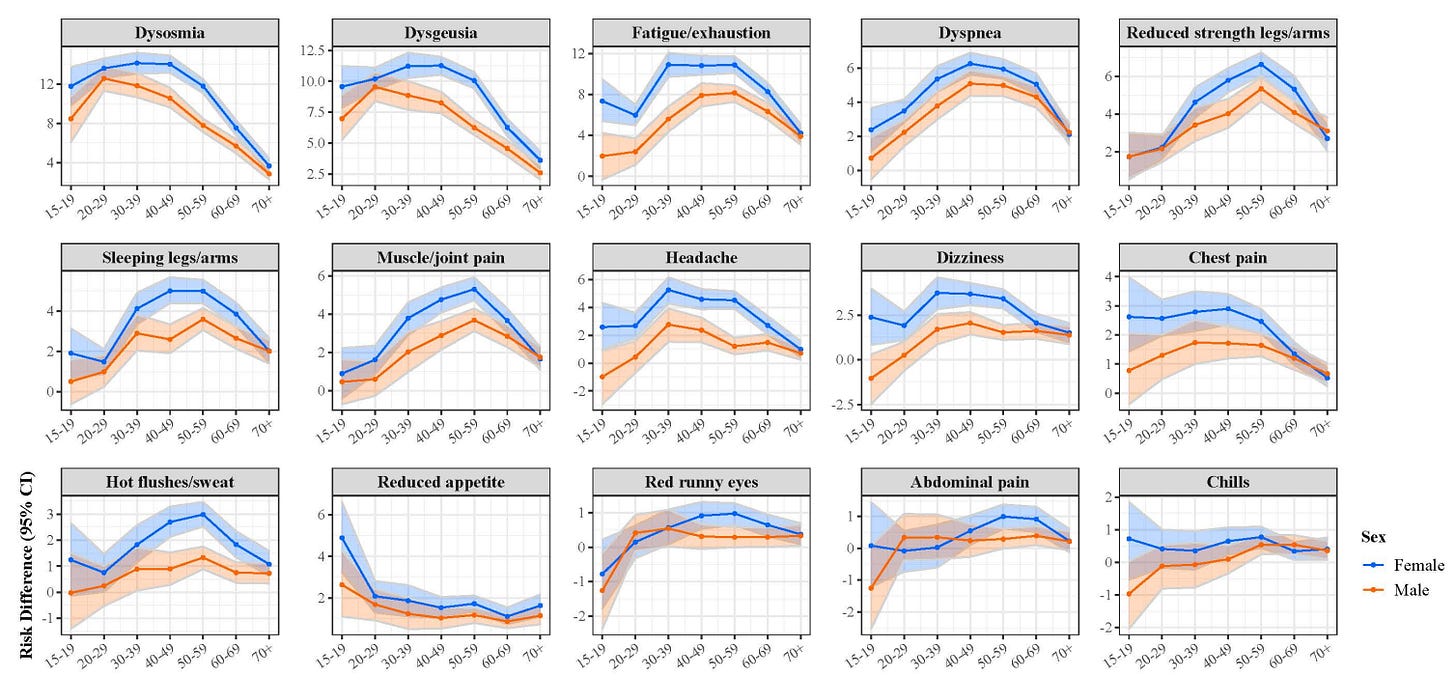
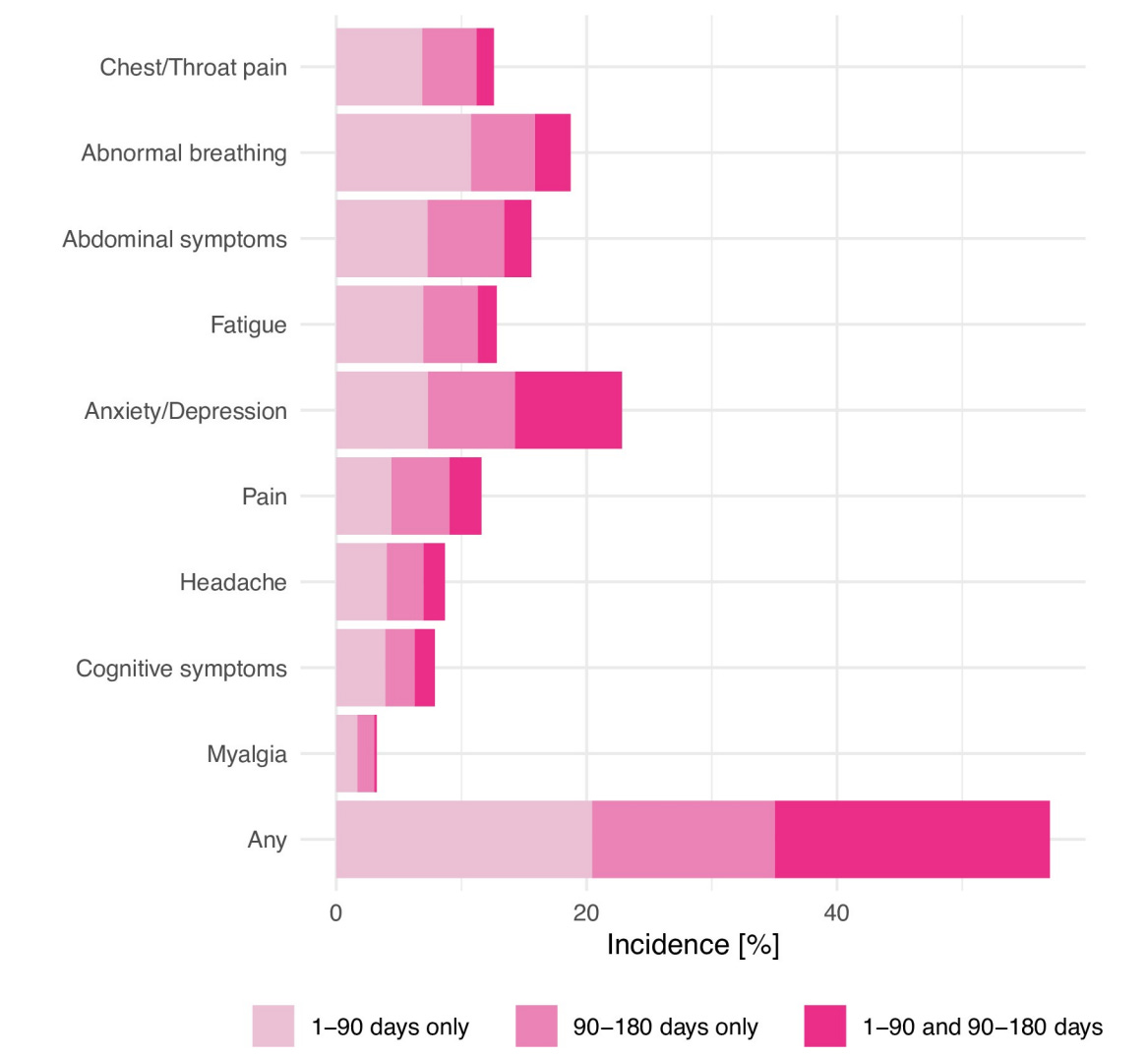
Symptoms also seem to depend on time since infection. In one robust U.S. study, the most common symptoms in the first 90 days were different from the most common symptoms in the 90-180 days after infection.
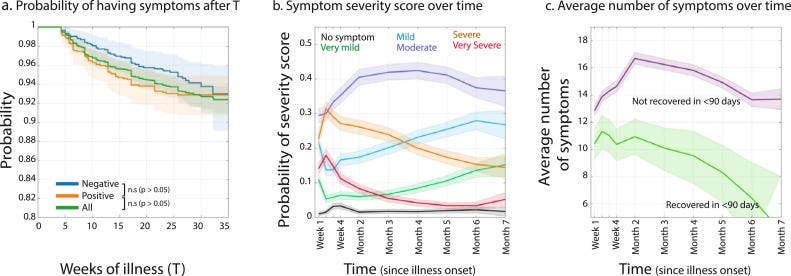
Symptoms can also fluctuate. 2 in 5 people with long COVID don’t have symptoms within the first 90 days. In other words, in a large proportion of people, symptoms popped up randomly 3 months after infection. A study in The Lancet found that severe long COVID, though, is not as likely to randomly pop up over time.
Symptoms can range from mild to debilitating. In the U.K., 65% of people report that long COVID reduced their ability to undertake day-to-day activities (see figure below). In the U.S., long COVID has resulted in 1.1 million Americans not working at any given time and another 2.1 million workers reducing hours rather than taking time off.
How long do symptoms last?
Unfortunately, we don’t know how long symptoms last because we are at the mercy of time. Symptoms subside for some after 30 days, some after 90 days, and others still have symptoms after two years. For example, a multicenter study of people with lost taste and smell found that at 2 months, 75–80% of people had regained these senses, and at 6 months, 95% had recovered them. In a sample of international long COVID patients, 91% still had symptoms after 6 months.
For the vast majority of people, we don’t think symptoms will last forever. In other post-viral syndromes, the majority of people eventually recover and are able resume their lives.
How does this compare to other viruses?
Lingering symptoms is not unique to SARS-CoV-2. We see this phenomenon with other viruses, including SARS, MERS, and the flu. Scientists have been busy assessing whether long COVID is due to SARS-CoV-2 itself or just a general consequence of a viral infection in general. This knowledge will help develop effective treatments.
Three solid studies have compared the presence and symptoms of long COVID to post-viral influenza (here, here, here). All three found that long COVID is more common and more severe than post-viral influenza. In one U.S. study, post-viral symptoms were 65% higher after SARS-CoV-2 than the flu.

Bottom line
Long COVID is common and broad in its impact on the body, making it incredibly difficult to diagnose and study. What is clear, though, is that this is a major public health problem and will continue to contribute to the health footprint of SARS-CoV-2 for years to come.
Tomorrow I will dive into the impact of long COVID19 on one organ system in particular. Stay tuned!
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, biostatistician, professor, researcher, wife, and mom of two little girls. During the day she has a research lab and teaches graduate-level courses, but at night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members. To support the effort, please subscribe here:







I have one quibble with this post. You said, "For the vast majority of people, we don’t think symptoms will last forever. In other post-viral syndromes, the majority of people eventually recover and are able resume their lives."
There is a lot of overlap between ME and Long COVID. As someone who's 35+ years into ME and who knows many people who are 20+ years into it, I cannot understand why anyone thinks Long COVID symptoms won't last forever. Recovering from ME is unusual. Most of us claw our way up to a point where we can resume some activities, but the ME does not go away and our capacity is diminished from what it should be. I am the highest functioning ME patient I've ever come across. At my best, I got to about 80%. I'm not there any more. Some of us are housebound or bedbound for the rest of our lives. A few of us die of ME.
If you prefer to ignore ME as a parallel (and it is indeed not a perfect parallel), we can look at the brain injuries so clearly documented by the UK biobank brain scan study and see that recovery from that damage is unlikely. Partial reclamation of some function, yes, as cells that are damaged but not destroyed rebound. Recovery, no.
So it's nice to believe that most Long COVID patients will eventually recover enough to resume a more or less normal life, but what evidence we have strongly suggests reality will not be that nice.
Aside from that... Thank you so very much for all the work and thought you put into these posts. I do appreciate your willingness to share your knowledge & expertise, and don't want this comment to cause you to think I don't.
Just want to thank you for all you are doing...these are great, must-reads that I share within my organization